A Natural Prescription: Exercise as a Key Therapy for Type 2 Diabetes
Each movement is a bloom of vitality—like flowers dancing in the spring breeze. Exercise is more than just physical effort; it’s a cornerstone of managing type 2 diabetes (T2DM) and a powerful tool for long-term health.
Globally, over 537 million adults live with diabetes, and over 90% of these cases are T2DM. In China alone, more than 140 million people are affected. The disease burden is immense—not just for individuals, but for healthcare systems. However, research consistently shows that structured physical activity improves insulin sensitivity, lowers blood glucose, enhances cardiovascular health, and even modulates gut microbiota.
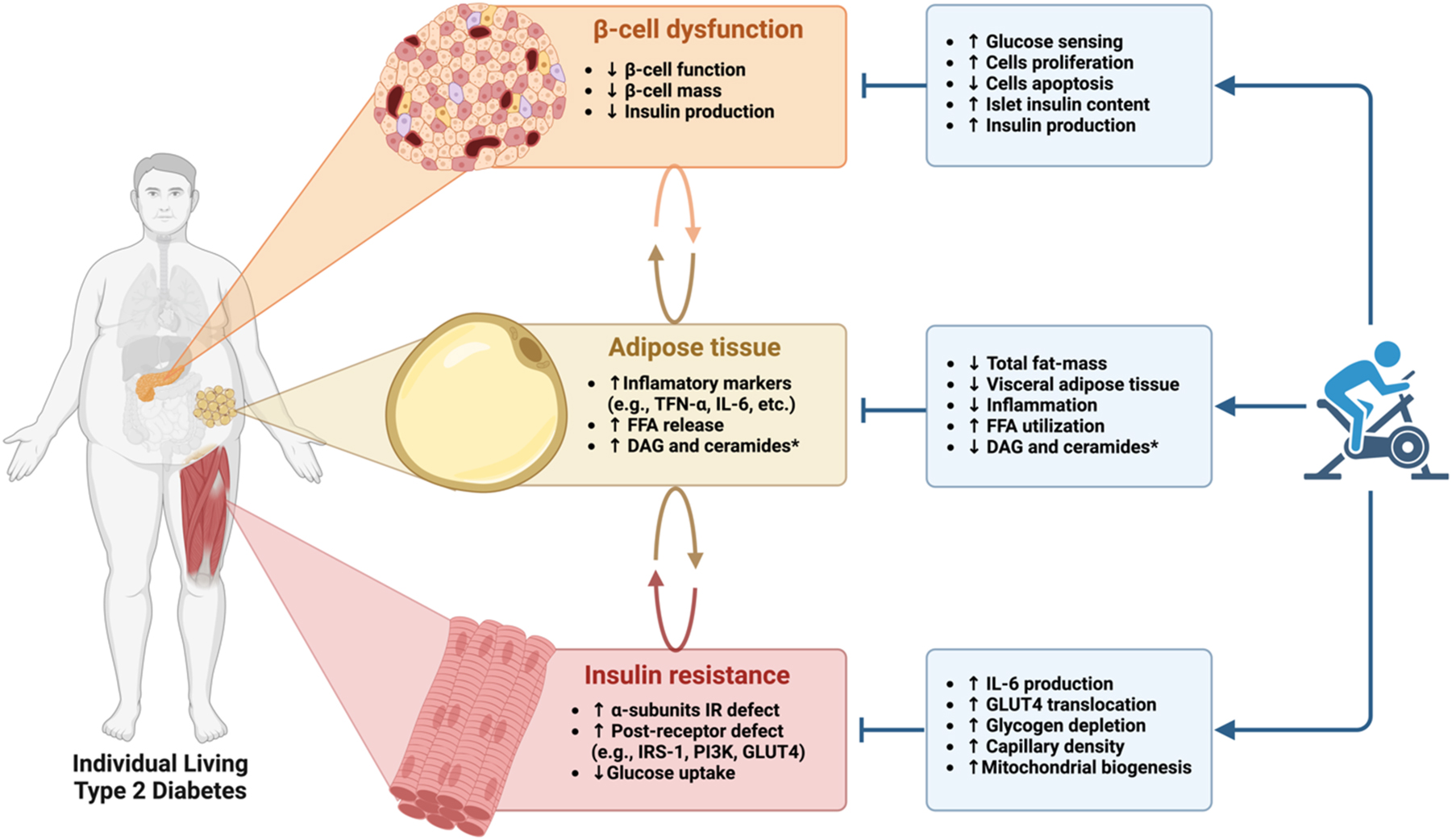
Why Exercise Matters for T2DM Management
Unlike medications, exercise doesn't just control symptoms—it can reverse pathophysiological mechanisms. Benefits of regular physical activity include:
- Improved insulin sensitivity
- Lower blood glucose levels (including HbA1c reductions of 0.4–0.9%)
- Better lipid profiles and blood pressure control
- Reduced body fat and improved muscle strength
- Lower cardiovascular risk and enhanced quality of life
Exercise is essential across all disease stages—from prevention to management. When used in combination with dietary changes and medications, it becomes a powerful strategy in integrated diabetes care.
Essential Terminology for Diabetes and Exercise
To understand and apply exercise recommendations, it’s important to clarify key terms:
- Physical Activity (PA): Any skeletal muscle movement that increases energy expenditure beyond rest (e.g., walking, gardening, cleaning).
- Exercise: A planned, structured subset of PA intended to improve fitness.
- Cardiorespiratory Fitness (VO₂max): A measure of aerobic capacity, directly tied to longevity.
- MET (Metabolic Equivalent): Used to quantify exercise intensity. Moderate-intensity = 3–5.9 METs.
- Resistance Training: Strength-based activity using bodyweight or equipment (e.g., dumbbells, bands).
- High-Intensity Interval Training (HIIT): Short bursts of intense effort alternated with rest periods, effective in reducing post-meal glucose spikes.
- Cool-down & Warm-up: Crucial to reduce injury risk and manage heart rate fluctuations.
Pre-Exercise Assessment for T2DM Patients
Not every patient is ready to jump into high-intensity workouts. A pre-exercise evaluation is essential and may include:
- Medical Review: Blood glucose trends, cardiovascular history, existing complications (e.g., retinopathy, neuropathy).
- Risk Screening Tools: Such as the Physical Activity Readiness Questionnaire (PAR-Q+).
- Fitness Testing: Includes VO₂peak, muscle strength (grip or 6-RM test), balance, and flexibility assessments.
Tailoring the Exercise Prescription for T2DM
A well-balanced exercise plan for T2DM patients should combine:
- Aerobic Exercise Frequency: 3–7 days/week Intensity: Moderate to vigorous (e.g., brisk walking, cycling) Duration: 150+ minutes/week Tip: 30-minute sessions or multiple 10-minute blocks Benefit: Decreases HbA1c by up to 0.7%
- Resistance Training Frequency: 2–3 days/week Repetitions: 8–10 reps, 1–3 sets Intensity: Start with 20–50% 1-RM Tools: Dumbbells, resistance bands, or bodyweight Benefit: Preserves muscle mass, improves glucose uptake
- Flexibility and Balance Training Frequency: 2–3 days/week Forms: Stretching, yoga, tai chi, or balance drills Benefit: Enhances mobility and reduces fall risk
- Interrupting Sedentary Time Tip: Stand or walk for 3 minutes every 30 minutes Benefit: Improves postprandial glucose and triglyceride levels
- HIIT (Optional for Advanced or Younger Patients) Structure: 10–60 seconds of high-intensity effort + recovery Caution: Screen for cardiovascular risk before starting Benefit: Rapid improvement in insulin sensitivity
Traditional Eastern Exercises for T2DM
Tai Chi and Baduanjin are considered moderate-intensity exercises. Practicing 3 times per week for 40 minutes per session can reduce HbA1c by approximately 0.4%. These are ideal for older adults or individuals new to exercise.
Additional Considerations
- Timing Matters: Post-meal exercise, especially 30–60 minutes after eating, reduces glucose spikes.
- Hydration: Maintain adequate water intake before, during, and after exercise.
- Injury Management: Use RICE protocol (Rest, Ice, Compression, Elevation) for minor injuries.
- Continuous Glucose Monitoring (CGM): Helps identify hypoglycemia risks during and after exercise.
Conclusion: Move to Improve
Exercise is not a secondary option—it’s frontline therapy for T2DM. With the right plan, supervision, and motivation, patients can significantly improve glycemic control and overall well-being.
Whether it's a walk in the park, a yoga session, or structured interval training, every step counts. Talk to your healthcare provider today to craft a safe and effective exercise plan tailored to your needs.
Categories: health