Advances in Insomnia Treatment and Drug Development
"Give yourself hope each day—not for tomorrow’s worries, nor yesterday’s regrets, but for a better today."
What Is Insomnia? Understanding the Definition and Diagnosis
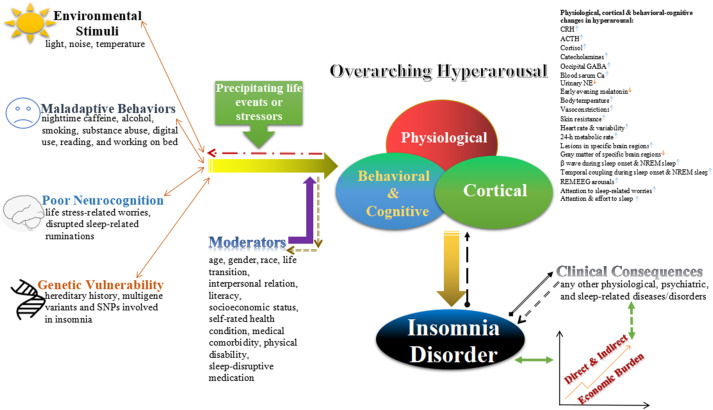
Insomnia, one of the most common sleep disorders, is defined as difficulty falling or staying asleep despite having adequate opportunities and environments for rest. It is diagnosed when poor sleep occurs at least three times per week and causes daytime impairments such as fatigue, mood swings, poor concentration, or physical discomfort.
Symptoms include:
- Trouble falling asleep (sleep latency >30 minutes)
- Frequent nighttime awakenings (≥2 times)
- Early morning awakenings
- Poor sleep quality and duration (typically <6.5 hours)
Notably, individuals who sleep less but function normally during the day should not be diagnosed with insomnia. The diagnosis is only valid when sleep issues are not better explained by other sleep disorders, mental health conditions, or medication side effects.
ICSD-3 Classification
According to the International Classification of Sleep Disorders, Third Edition (ICSD-3), insomnia is classified into:
- Chronic Insomnia (lasting ≥3 months)
- Short-term Insomnia (lasting <3 months)
- Other Insomnia (not meeting criteria above, used cautiously)
Epidemiology and Market Overview
A meta-analysis of 17 studies in China estimated the insomnia prevalence at 15% among the general population using PSQI or AIS scores. During the global COVID-19 pandemic, the prevalence surged globally to 20–45%, with one Chinese survey reporting 29.2%.
Insomnia impairs quality of life, work performance, and increases the risk of accidents and chronic diseases. In 2024, the global insomnia treatment market was valued at USD 2.26 billion, projected to grow at a CAGR of 8.1% through 2029.
In China, sales of sedative-hypnotic drugs reached RMB 22.3 billion in the first half of 2024 across public hospitals and pharmacies.
Treatment Goals and Modalities
Primary Goals:
- Improve sleep quality and duration
- Prevent progression to chronic insomnia
- Reduce comorbid physical or mental health risks
- Restore daytime function and quality of life
- Minimize side effects from treatment
Treatment Options:
- Pharmacological Therapy Short-term relief with caution for side effects and dependence
- Cognitive Behavioral Therapy for Insomnia (CBT-I) Gold standard for long-term management
- Physical Therapies Including light therapy, transcranial magnetic stimulation (TMS), electrical stimulation, and biofeedback
- Traditional Chinese Medicine (TCM) Widely practiced, yet needs evidence-based validation
- Complementary Therapies E.g., aromatherapy, dietary adjustments, massage
Current Medications for Insomnia
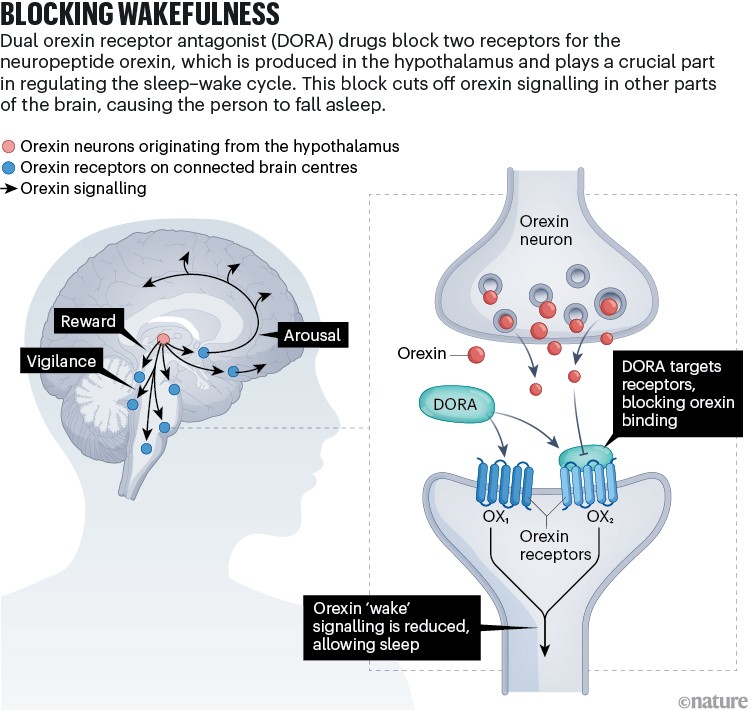
A variety of prescription medications are used, including benzodiazepines, non-benzodiazepine hypnotics (Z-drugs), melatonin receptor agonists, orexin receptor antagonists, and herbal sedatives. Each has its benefits, indications, and risk profile.
Note: Long-term use of sedative-hypnotics is associated with tolerance, dependence, and adverse effects. Use under medical supervision.
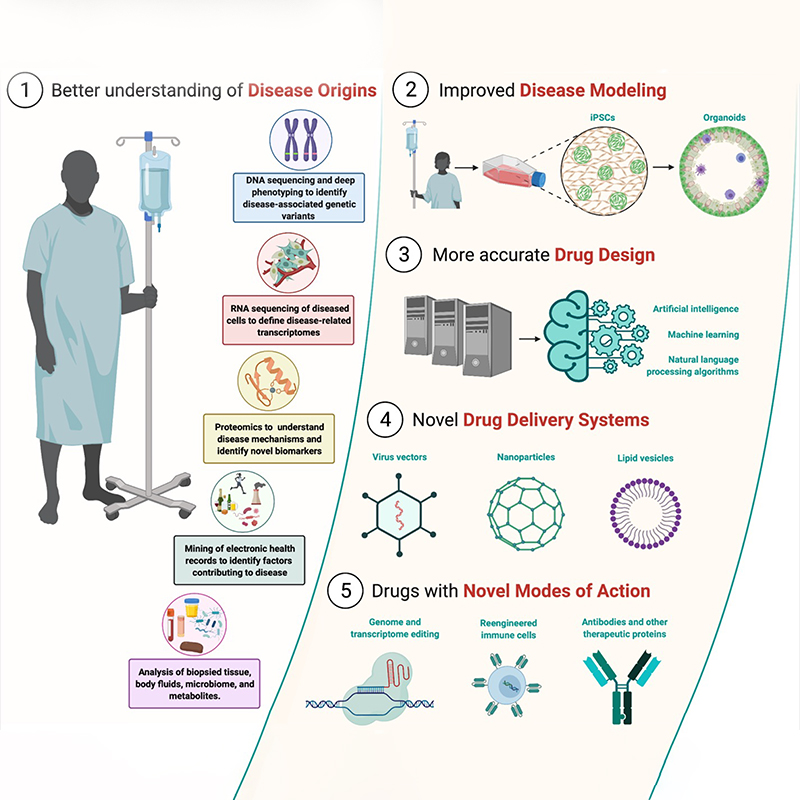
Recent Advances in Drug Development
R&D Highlights (as of October 2024):
- Over 10 global pharma companies have launched insomnia drugs, including Eisai, Pfizer, Sanofi, and Idorsia.
- Top drug targets: GABA-A receptors, histamine H1, orexin receptors, melatonin receptors
1. Daridorexant Hydrochloride
A dual orexin receptor antagonist (DORA) approved in the U.S. in 2022; blocks wake-promoting neuropeptides without causing addiction.
- Developer: Idorsia
- China Status: NDA accepted by NMPA in July 2024
- Advantage: Improves sleep without sedation or withdrawal
2. Didasemin (地达西尼)
Approved in China in November 2023, this benzodiazepine partial agonist targets GABA-A receptors.
- Indication: Short-term treatment of insomnia
- Dose: 2.5 mg nightly, not exceeding 4 weeks
- Caution: Monitor for dependence, especially in patients with a history of substance abuse
3. Tasimelteon
A melatonin receptor agonist approved by the U.S. FDA for circadian rhythm sleep disorders.
- Improves sleep latency and quality, ideal for patients with sleep apnea or COPD
- Advantage: No respiratory suppression or withdrawal risk
Conclusion
Insomnia is a widespread and burdensome condition with profound impacts on personal health, productivity, and public safety. While behavioral and cognitive therapies remain the cornerstone of treatment, ongoing pharmaceutical innovations—especially those targeting novel mechanisms like orexin and melatonin receptors—offer promising alternatives with better safety profiles.
As science advances, patients and clinicians alike can look forward to more personalized and effective treatment options for achieving restful, restorative sleep.
Categories: health