Comprehensive Review of Diagnosis and Treatment for MAFLD (Metabolic Dysfunction-Associated Fatty Liver Disease)
Introduction
Metabolic dysfunction-associated fatty liver disease (MAFLD), previously known as non-alcoholic fatty liver disease (NAFLD), has become the most common chronic liver condition globally. In China, it has surpassed viral hepatitis as the leading cause of chronic liver disease. MAFLD encompasses a spectrum of hepatic conditions characterized by excess fat accumulation in the liver, typically caused by metabolic dysfunction. This article provides an in-depth review of MAFLD's definition, classification, risk factors, epidemiology, diagnostic criteria, and treatment options including lifestyle changes, pharmacotherapy, and surgical interventions.
1. Definition and Classification of MAFLD
MAFLD represents a heterogenous group of liver diseases influenced by genetic, epigenetic, dietary, and lifestyle factors. Clinically, fatty liver diseases are categorized into:
- MAFLD
- Alcohol-related liver disease (ALD)
- Secondary fatty liver diseases (e.g., due to medications or malnutrition)
- Mixed type fatty liver disease
- Cryptogenic fatty liver disease
MAFLD is characterized by hepatic steatosis (fat accumulation in ≥5% of hepatocytes) in conjunction with one or more of the following:
- Overweight/obesity
- Type 2 diabetes mellitus (T2DM)
- Evidence of metabolic dysregulation
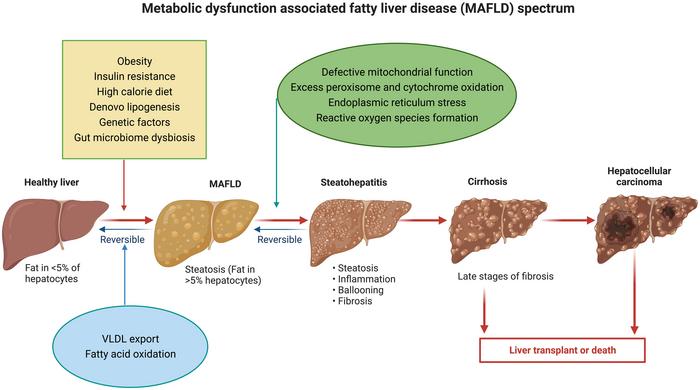
Disease Progression Stages:
- Simple fatty liver (MAFL)
- Metabolic-associated steatohepatitis (MASH)
- Liver fibrosis
- Cirrhosis
- Hepatocellular carcinoma (HCC)
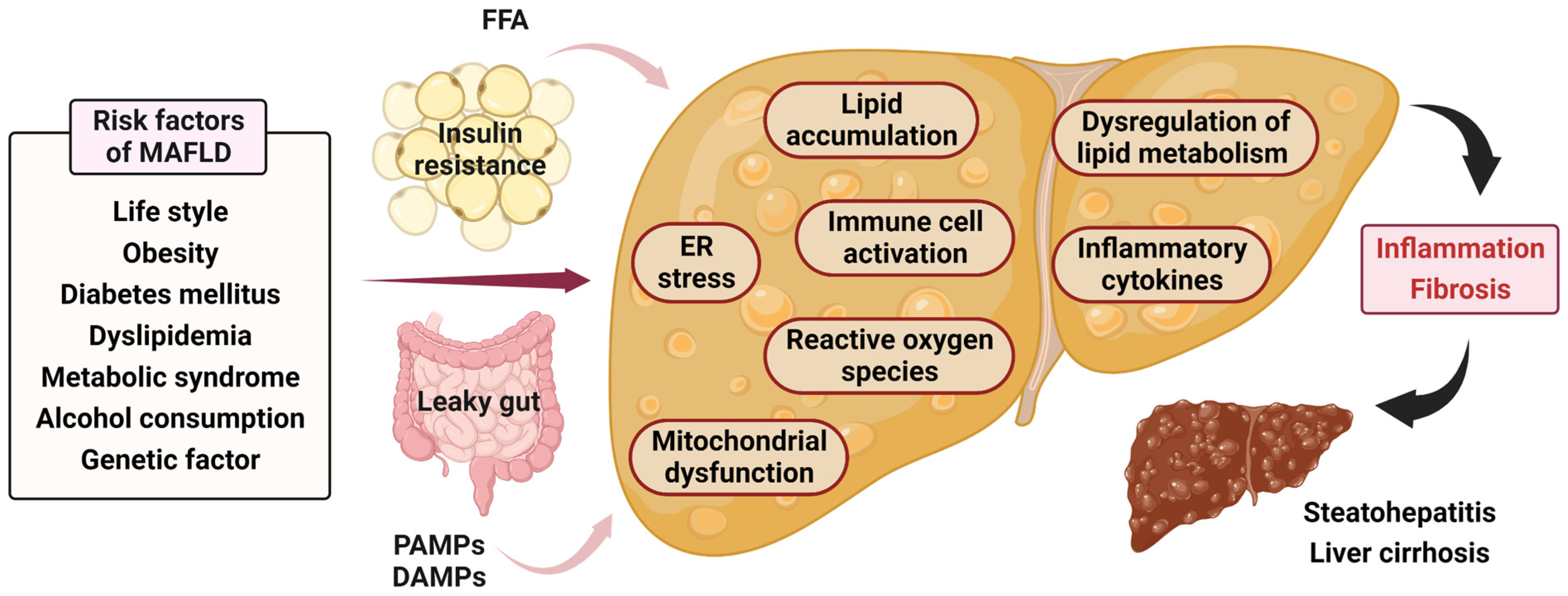
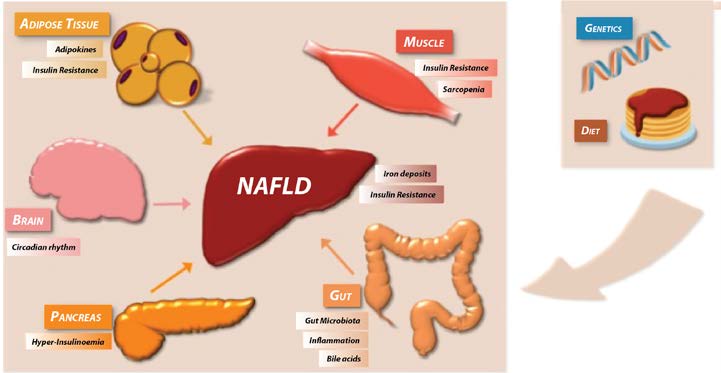
Primary Risk Factors:
- Obesity
- Metabolic syndrome (MetS)
- T2DM
- Sedentary lifestyle
- Unbalanced diet (e.g., high-sugar, high-fat intake)
2. Epidemiology of MAFLD
Global MAFLD prevalence is estimated at 32.4%. In Asia, it affects roughly 29.6% of the adult population, with increasing trends over the past two decades.
China-Specific Data:
- National average prevalence: ~29.9%
- Incidence rate: 56.7 per 1,000 person-years
- Highest provincial prevalence: Heilongjiang (50.48%)
- Lowest: Hainan (9.72%)
- Peak age group: 50-59 years
- Gender gap: Men (34.75%) > Women (23.50%); postmenopausal women (39.9%) > premenopausal women (19.5%)
Comorbidities:
- Obesity: 51.6% MAFLD prevalence
- T2DM: ~65% MAFLD prevalence; 31.5% MASH
- Hypertension increases MAFLD risk by ~1.7x
3. Diagnostic Criteria for MAFLD and MASH
MAFLD Diagnostic Criteria:
- Imaging or histological evidence of hepatic steatosis (via ultrasound, CAP, or biopsy)
- Presence of metabolic risk factors
- Exclusion of significant alcohol intake and other specific liver diseases
Key Diagnostic Tools:
- Ultrasound: Most common imaging technique for fatty liver
- CAP (controlled attenuation parameter): For non-invasive liver fat quantification
- LSM (liver stiffness measurement): For assessing fibrosis
- Liver biopsy: Gold standard for grading MASH and fibrosis
MASH Diagnostic Criteria:
- MAFLD diagnosis confirmed
- Liver biopsy shows steatosis ≥5%, hepatocyte ballooning, lobular or portal inflammation

4. Treatment Strategies for MAFLD
A. Lifestyle Modifications
1. Diet Therapy
- Caloric reduction: Men (1200-1400 kcal/day), Women (1000-1200 kcal/day)
- Minimum protein intake: 1.2g/kg/day to prevent muscle wasting
- Recommended diets:Mediterranean dietLow-carbohydrate dietIntermittent fastingJiangnan dietary pattern (rich in vegetables, whole grains, omega-3)
- Sodium intake: ≤2300 mg/day
- Increased water intake
2. Physical Activity
- Moderate-intensity aerobic exercise: ≥150 min/week
- High-intensity interval training (HIIT): 2-4 min bursts, 3-5x/week
- Improves insulin sensitivity, liver fat content, and cardiovascular fitness
3. Behavioral Changes
- Avoid alcohol, smoking, and erratic eating habits
- Encourage regular meals and sufficient sleep
- Coffee consumption (>3 cups/day) associated with reduced HCC risk
B. Pharmacological Treatments
1. Weight Loss Medications
- Indicated for BMI >28 kg/m2 if lifestyle interventions fail after 3 months
- Approved agents: Orlistat, Liraglutide, Semaglutide, Benaglutide
- Bariatric surgery: Considered for non-cirrhotic patients meeting criteria
2. Antidiabetic Agents
- GLP-1 receptor agonists (e.g., Liraglutide, Semaglutide): Reduce liver fat, inflammation, and cardiovascular risk
- SGLT2 inhibitors (e.g., Dapagliflozin): Improve insulin resistance, reduce ALT levels
- Pioglitazone: Beneficial for prediabetes and T2DM patients with MASH
3. Lipid-Lowering Drugs
- Statins: Safe and effective, especially in compensated liver disease
- Alternatives: Ezetimibe, PCSK9 inhibitors for statin-intolerant patients
- Fibrates: For TG >5.6 mmol/L, to prevent pancreatitis
4. Antihypertensives
- First-line: ACE inhibitors or ARBs
- Target BP: <130/85 mmHg
- Additional options: CCBs, beta-blockers (e.g., carvedilol), diuretics
5. Liver-Specific Therapies
- Vitamin E (800 IU/day): For non-diabetic, non-cirrhotic MASH
- Investigational drugs:Resmetirom (THR-β agonist)Lanifibranor (PPAR pan-agonist)Efruxifermin (FGF21 analog)Tirzepatide (GLP-1/GIP dual agonist)
C. Surgical Options
1. Metabolic/Bariatric Surgery
- Techniques: Gastric bypass, sleeve gastrectomy, duodenal switch
- Results: Significant weight loss, improved T2DM and CV outcomes
2. Liver Transplantation
- For patients with decompensated cirrhosis or HCC due to MASH
- Comparable survival outcomes to other etiologies
5. Drug Development Landscape
As of July 2025, there are 1,023 drugs under development targeting MAFLD. Leading companies include Madrigal Pharmaceuticals, Zydus Lifesciences, Novo Holdings, and China Biopharma. Key investigational targets include:
- Thyroid hormone receptor-β
- PPAR-α/γ agonists
- GLP-1 receptors
- GCGR/GLP-1R dual agonists
- FGF21 receptors
These promising agents are at various clinical trial stages, with some like Resmetirom already approved in the US for significant fibrosis associated with MASH.
Conclusion
MAFLD represents a growing public health burden linked to the global epidemic of obesity and metabolic syndrome. Early diagnosis, lifestyle modification, targeted pharmacotherapy, and multi-disciplinary collaboration are key to effective management. Continued clinical trials and research are paving the way for novel therapeutics with better safety and efficacy profiles.
Stay tuned for our follow-up articles on integrative treatments, including Traditional Chinese Medicine options, and real-world patient management strategies.
Categories: health
