Diabetic Retinopathy: Causes, Stages, and the Latest Treatments for Vision Preservation
"Amid the vastness of life's challenges, serenity within is our strongest shield."
I. What Is Diabetic Retinopathy (DR)?
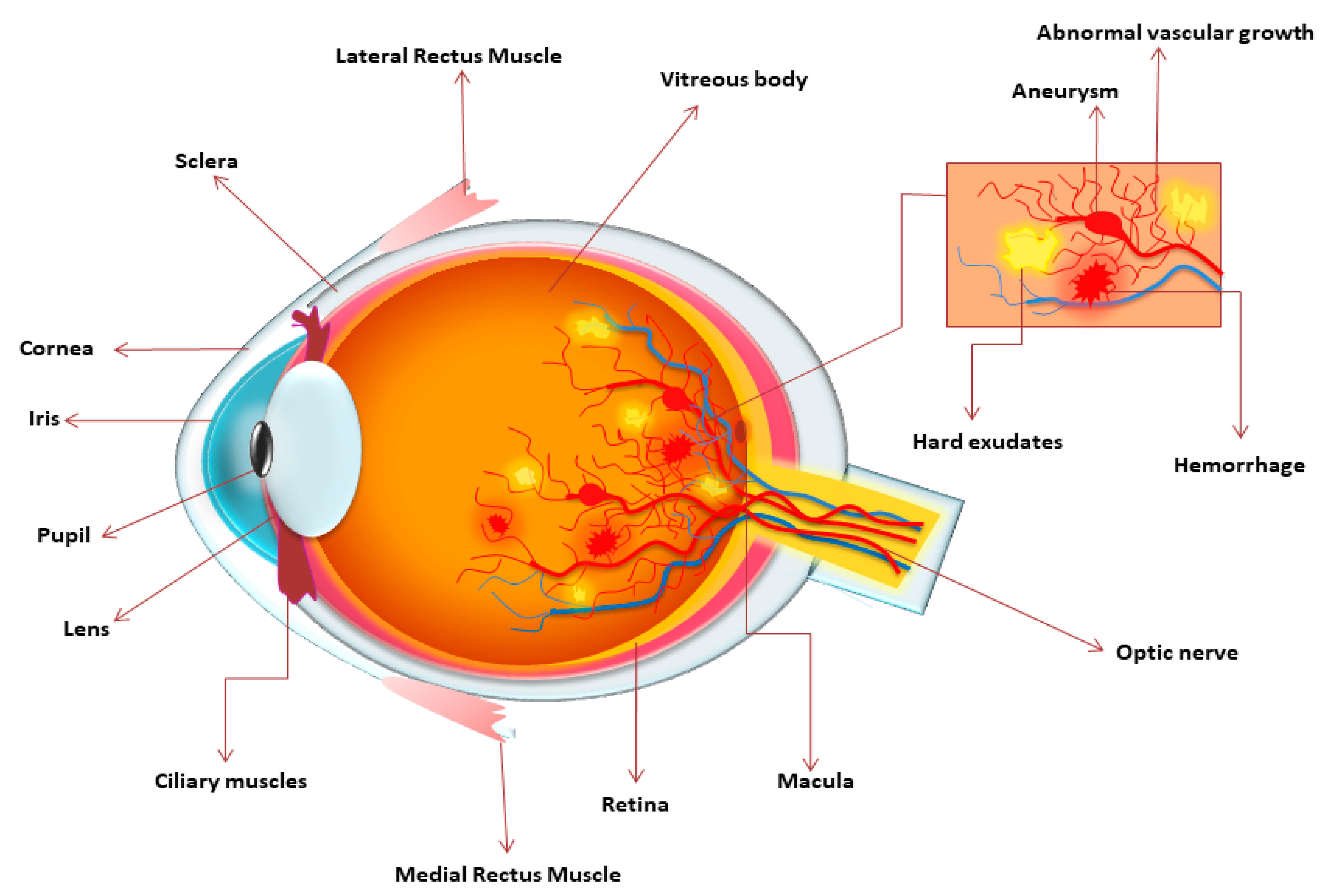
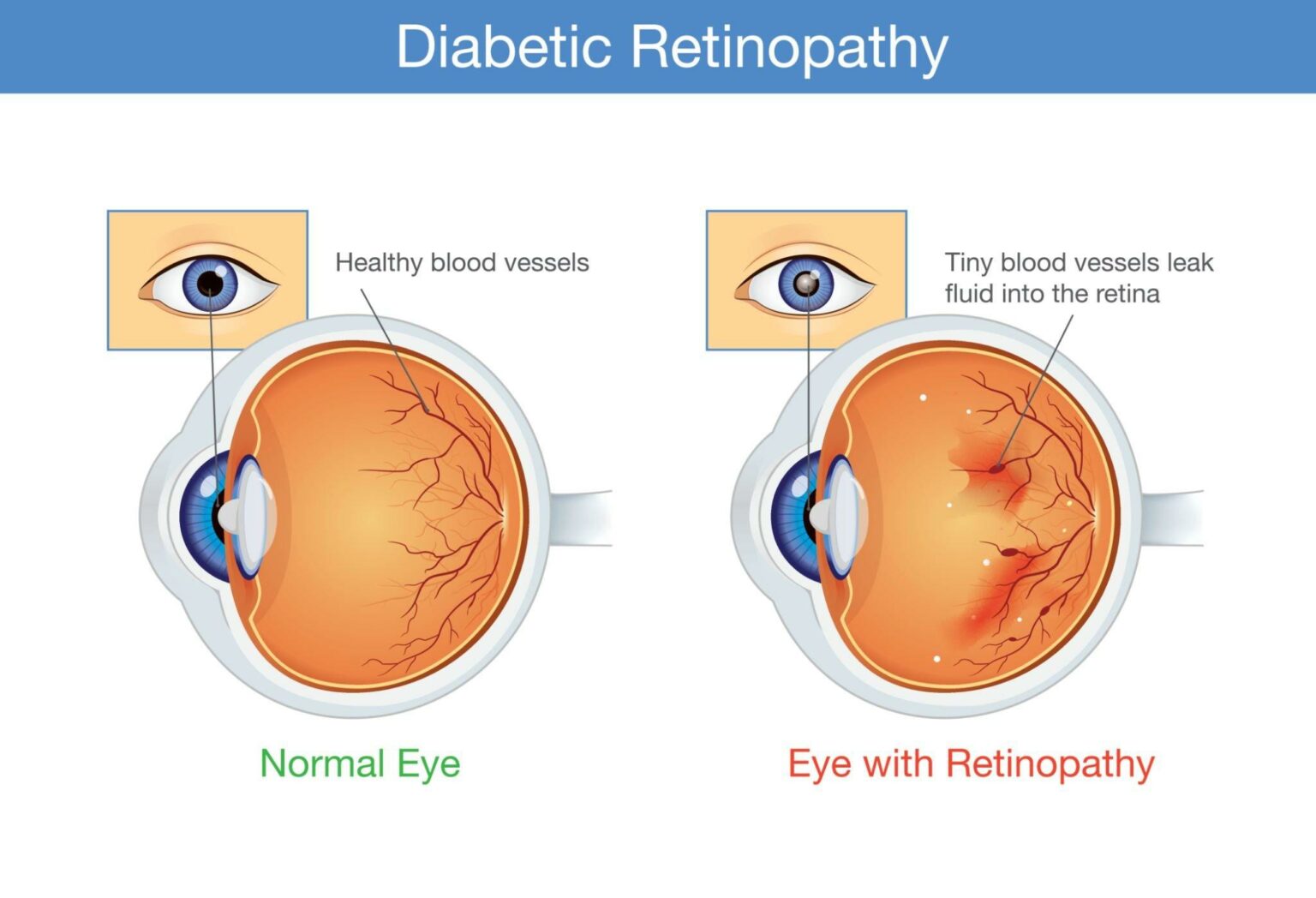
Diabetic Retinopathy (DR) is a common microvascular complication of diabetes and one of the leading causes of blindness in working-age adults globally. It is characterized by progressive damage to the small blood vessels of the retina due to chronic hyperglycemia. DR is often accompanied by neuroglial dysfunction and can result in irreversible vision loss if untreated.
II. Causes and Risk Factors
DR is primarily caused by prolonged high blood sugar levels which damage retinal capillaries. Key risk factors include:
- Duration of diabetes
- Poor blood glucose control
- Hypertension and dyslipidemia
- Insulin resistance, obesity, pregnancy, and genetic predisposition
- Smoking and subclinical hypothyroidism
III. Classification and Staging
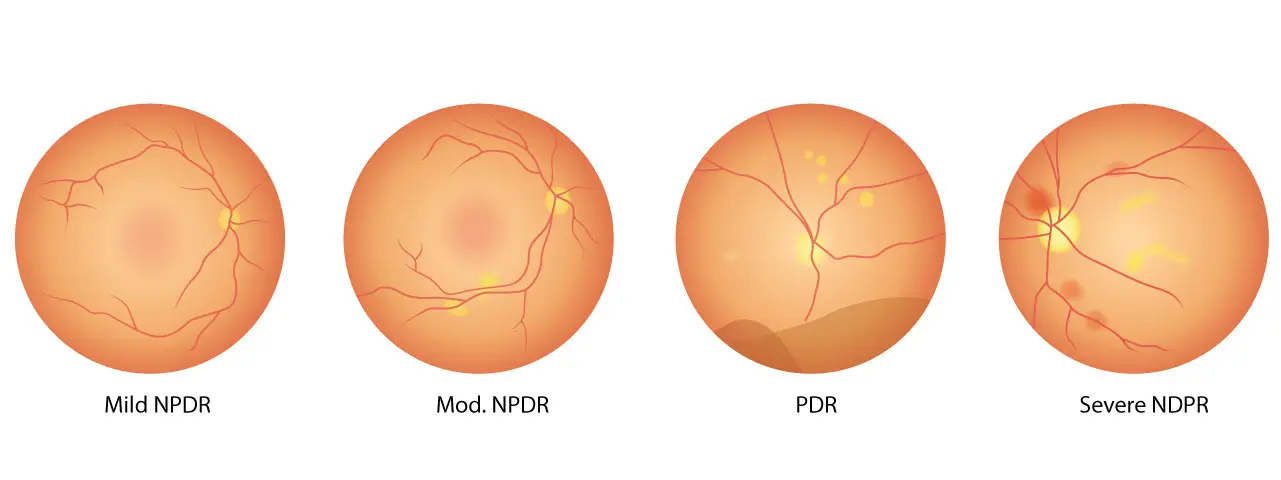
DR is categorized into:
- Non-Proliferative Diabetic Retinopathy (NPDR): Early stage with microaneurysms, hemorrhages, and cotton wool spots.
- Proliferative Diabetic Retinopathy (PDR): Advanced stage with abnormal new blood vessels (neovascularization), which may lead to vitreous hemorrhage and retinal detachment.
- Diabetic Macular Edema (DME): Can occur at any stage, caused by leakage of fluid from retinal capillaries affecting central vision.
NPDR Stages:
- Mild: Microaneurysms only
- Moderate: More extensive retinal abnormalities without meeting criteria for severe NPDR
- Severe: Hemorrhages in all quadrants, venous beading, or intraretinal microvascular abnormalities (IRMAs)
PDR Stages:
- Early PDR: Neovascularization on the disc (NVD) or elsewhere (NVE)
- High-Risk PDR: NVD >1/4 to 1/3 disc area or NVE >1/2 disc area with vitreous/preretinal hemorrhage
- Advanced PDR: Fibrovascular proliferation and tractional retinal detachment
DME Types:
- Non-Center-Involving (NCI-DME)
- Center-Involving (CI-DME)
IV. Epidemiology
According to the International Diabetes Federation (IDF), over 537 million adults (20–79 years) had diabetes in 2021, projected to rise to 783 million by 2045. An estimated 103 million adults globally had DR in 2020, expected to reach 160 million by 2045.
In China, DR prevalence among diabetics is around 22.4%, with higher rates in northern and rural areas. The highest prevalence is among individuals aged 50–59 years.
V. Diagnosis and Screening
A comprehensive ophthalmic evaluation includes medical history, visual acuity, intraocular pressure measurement, dilated fundus examination, and optical coherence tomography (OCT). Fundus photography (ETDRS 7-field or ultra-wide field imaging) helps in DR staging.
For systemic evaluation, it is essential to review diabetes duration, glycemic control, and comorbidities like hypertension and dyslipidemia.
VI. Treatment Strategies for Diabetic Retinopathy
Treatment includes both systemic management (glycemic, blood pressure, and lipid control) and ocular-specific interventions depending on DR stage and presence of DME.
1. Observation
- Mild to moderate NPDR without DME: Regular monitoring every 6–12 months.
- With CI-DME and vision loss: Anti-VEGF injections recommended.
2. Laser Photocoagulation (PRP)
Panretinal photocoagulation is a cornerstone for high-risk PDR and severe NPDR. It reduces the risk of severe vision loss. When DME coexists, anti-VEGF is often administered before PRP.
3. Anti-VEGF Therapy
Intravitreal anti-VEGF agents are first-line treatments for DME and effective in reducing neovascularization in PDR. Common drugs include:
- Ranibizumab: Humanized monoclonal antibody fragment (Fab) targeting all VEGF-A isoforms.
- Conbercept: Fusion protein targeting VEGF-A, VEGF-B, and PlGF.
- Aflibercept: VEGF and placental growth factor (PlGF) inhibitor.
These drugs effectively reduce vascular leakage, promote visual improvement, and delay disease progression.
4. Corticosteroid Therapy
Used when anti-VEGF response is inadequate. Options include:
- Dexamethasone intravitreal implant (Ozurdex): Biodegradable, sustained-release steroid.
- Triamcinolone acetonide (TA): Off-label use for DME.
Steroids modulate inflammation and help restore the blood-retinal barrier.
5. Vitrectomy (PPV)
Indicated in:
- Non-resolving vitreous hemorrhage
- Tractional retinal detachment
- Proliferative membranes
Combining PPV with anti-VEGF enhances outcomes. Not first-line for DME unless traction or severe non-resolving edema persists.
6. DME with Cataract
Diabetic patients are more prone to early-onset cataracts. Pre-operative DR stabilization is essential. If DME is present, treat with anti-VEGF or corticosteroids concurrently with cataract surgery.
VII. Emerging Therapies and Drug Development
As of July 2025, over 452 drugs are under development for DR. Key players include:
- Top 5 Companies: Novartis, Roche, LuFa Pharma, Samsung Biologics, STADA
- Top 5 Targets: VEGF-A, PGF x VEGF-A, GR, VEGFR2, Ang2 x VEGF-A
These developments promise safer and more effective treatments for DR in the future.
Conclusion
Diabetic Retinopathy is a major threat to vision but is manageable with early diagnosis, comprehensive treatment, and regular follow-up. Integrated systemic and ocular therapies, along with advancements in pharmacology, offer hope for preserving sight in diabetic individuals.
Let awareness lead to action—because every blink is worth protecting.
Categories: health